Pages connexes
Europe
Page Organisation et financement en France Page Parcours et programmes de soins Résumé en français du rapport du centre fédéral d’expertises belge de 2007 – Le rapport
Présentations / Articles
Modèles internationaux
Quality and Outcome Measures for Rehabilitation Programs Carl V Granger, Rene Cailliet, MD (en pdf) Site MEDPAC: Post-acute care – Payments basics Comparaison des paiements en post-aigu France-USA
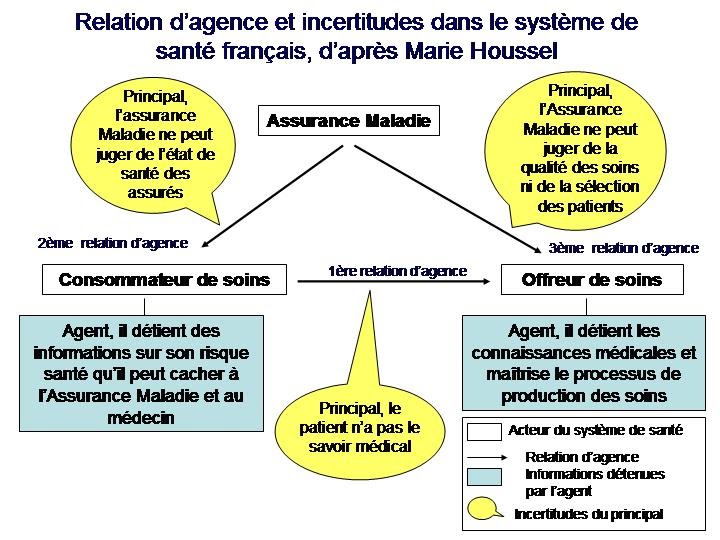
Relation d’agence d’après Marie Houssel
Cost-efficiency of specialist hyperacute in-patient rehabilitation services for medically unstable patients with complex rehabilitation needs: a prospective cohort analysis BMJ Open 2016;6:e012112 doi:10.1136/bmjopen-2016-012112
Payment by Results for Rehabilitation – Update (as per19.7.10) Lynne Turner-Stokes
Healthcare tariffs for specialist inpatient neurorehabilitation services: rationale and development of a UK casemix and costing methodology Lynne Turner-Stokes – Stephen Sutch – Robert Dredge Clin Rehabil 2012 26: 264
Engaging the hearts and minds of clinicians in outcome measurement – the UK rehabilitation outcomes collaborative approach Turner Stokes et al.
Healthcare resource groups
Autres documents saillants
Medical rehabilitation in 2011 and beyond – Report of a joint working party of the Royal College of Physicians and the British Society of Rehabilitation Medicine November 2010 BSRM Standards for Rehabilitation Services Mapped on to the National Service Framework for Long-Term Conditions Britih society of rehabilitation medicine (position papers, core standards and guidelines)
|
Méthodologie de regroupement des patients en réadaptation – Rehabilitation Patient Group (RPG) Grouping Methodology and Weights National Rehabilitation Reporting System: Case Mix Rehabilitation Patient Group Resource Materials and Frequently Asked Questions, 2013–2014 Méthodologie de regroupement GPR et pondérations des coûts en réadaptation
Système national d’information sur la réadaptation
L’outil de recueil: métadonnées de la Système national d’information sur la réadaptation (SNIR) (fiche d’admission, de sortie et de suivi) National Rehabilitation Reporting System (NRS) Metadata
Les groupes clients
« Les gestionnaires des soins de santé, cliniciens et autres professionnels de la santé au Canada doivent relever un défi de plus en plus difficile : réduire les coûts tout en maintenant ou améliorant la qualité et l’accès aux soins. Dans un tel contexte, l’information que les décideurs utilisent pour gérer les établissements de santé et les régies régionales est plus importante que jamais. Nous avons donc pris l’initiative d’élaborer et de mettre en œuvre des méthodologies de regroupement des clients. Celles-ci classent les patients dans des groupes homogènes sur les plans statistique et clinique selon les données cliniques et administratives recueillies. Il faut comprendre les différents besoins des patients et clients avant de pouvoir comparer les organismes de santé et l’utilisation des ressources en fonction des groupes clients. » Michel Coulmont, Chantal Roy, Patrick Fougeyrollas
|
La réorganisation des services posthospitaliers de convalescence et de réadaptation
A conceptual framework for the analysis of health care organizations’ performance. Sicotte C, Champagne F, Contandriopoulos AP, Barnsley J, Béland F, Leggat SG, Denis JL, Bilodeau H, Langley A, Brémond M, Baker GR. Health system performance http://www.cihi.ca/CIHI-ext-portal/internet/en/document/health+system+performance/indicators/health/indic_def_health_system_12
Plan de mesure Réadaptation – 2011 (Association nationale pour le développement de qualité dans les hôpitaux et les cliniques)
http://www.isesuisse.ch/fr/conferences/conf_0805_pcs-hansenberger-f-23.pdf
Réadaptation médicale: situation Situation et avenir du financement en Allemagne http://www.isesuisse.ch/fr/conferences/conf_0805_pcs-neubauer-f-23.pdf
| Payments basics (MEDPAC) Home health care services payment system 10/14/2016 Document Type: Payment Basics Hospice services payment system 10/14/2016 Document Type: Payment Basics Inpatient rehabilitation facilities payment system 10/14/2016 Document Type: Payment Basics Long-term care hospitals payment system 10/14/2016 Document Type: Payment Basics Skilled nursing facility services payment system 10/14/2016 Document Type: Payment Basics | Une réforme des soins post-aigus est en cours vers un système uniforme de données et de paiement.Post-Acute Quality Initiatives: The Continuity Assessment Record and Evaluation (CARE) Item SetIRF – PAI (Inpatient Rehabilitation Facilities)MDS 3.0 (Skilled Nursing Facilities, …)Aux USA outils de recueil et de tarification sont différents selon le type de soins post-aigus |
Post-Acute Care Payment Reform Demonstration: Final Report
Developping a unified payment system for post-acute care Post-Acute Care Reform — Beyond the ACA The Value of AHA Membership for Long-term and Post-acute Care Providers Reject Proposals to Equalize Payments for Inpatient Rehabilitation Hospitals and Units and Skilled Nursing Facilities for Certain Services (AHA) IMPACT Act of 2014 Data Standardization & Cross Setting Measures
|
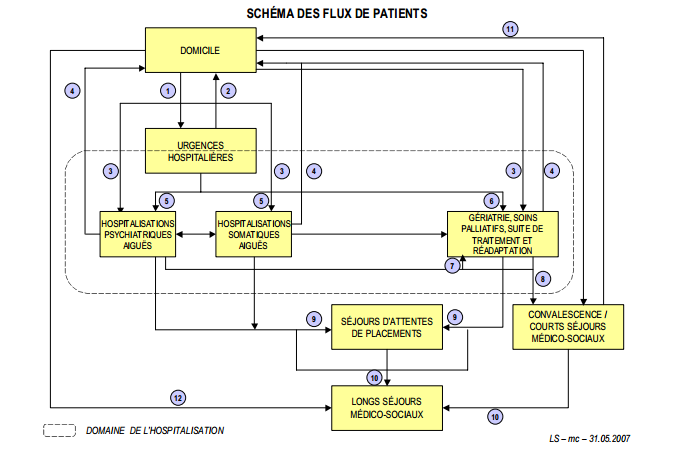
Schéma des parcours de soins aux USA
Final Report. Cheryl l. Damberg, Melony E. Sorbero, Peter S. Hussey, Susan Lovejoy, hangsheng liu, and ateev mehrotra
February 2009 – Assistant Secretary for Planning and Evaluation U.S. Department of Health and Human Services
|
| Quality and Outcome Measures for Rehabilitation Programs. Author: Carl V Granger, MD; Chief Editor: Rene Cailliet, MD (télécharger en pdf)
Imprimer l’ensemble du document: cliquer sur imprimer et sur « print the entire content »
« Currently, the third-party payer is exerting a force on how services are rendered and on the types of outcomes that can be expected. Thus, it is incumbent upon the clinician to balance the benefit of treatment with its cost, while taking into account perceptions of the value of the treatment from the viewpoint of the payer, patient, family, and community » » UDSMR applies scientific research to the process of assessment of outcomes. The goal is to improve patient care and function by (1) identifying the patterns of disability and recovery and (2) providing appropriate and timely feedback to clinicians so they can promote effective and efficient care for the patient. » … « The more we study function in a systematic fashion, the more it is evident that function transcends everything. As we function, so shall we live. » Carl V Granger Medicare Program; Inpatient Rehabilitation Facility Prospective Payment System for Federal Fiscal Year 2014 U.S. Department of Health and Human Services Centers for Medicare & Medicaid Services (CMS) Report to Congress: Post Acute Care Payment Reform Demonstration (PAC-PRD) January 2012 http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/downloads/Flood_PACPRD_RTC_CMS_Report_Jan_2012.pdf Exploring Episode-Based Approaches for Medicare Performance Measurement, Accountability and Payment – Final Report. Février 2009 http://aspe.hhs.gov/health/reports/09/mcperform/report.shtml Post-Acute Care Episodes Expanded Analytic File – Final Report – April 2011 – Prepared for: Susan Bogasky Assistant Secretary for Planning and Evaluation (ASPE) U.S. Department of Health and Human Services Hubert H. Humphrey Building, Room 443F5 200 Independence Avenue, SW Washington, DC 20201 http://aspe.hhs.gov/health/reports/2011/PACexpanded/index.shtml Top 10 Parameters for Determining a Post-acute Care Strategy http://www.thecamdengroup.com/thought-leadership/blog/top-10-parameters-for-determining-a-post-acute-care-strategy/ Post-Acute Care of the Elderly Patient Rehabilitation and Transitions of care http://www.docstoc.com/docs/62291502/Post-Acute-Care-of-the-Elderly-Patient-Rehabilitation-and Rationale and principles of early rehabilitation care after an acute injury or illness GEROLD STUCKI1,2, MARITA STIER-JARMER , EVA GRILL , & JOHN MELVIN Department of Physical Medicine and Rehabilitation, Ludwig-Maximilians-University, Munich, Germany, ICF Research Branch of the WHO FIC Collaborating Center (DIMDI), IMBK, Ludwig-Maximilians-University, Munich, Germany, and Department of Rehabilitation Medicine, Jefferson Medical College, Thomas Jefferson University, Philadelphia, USA http://knowledgetranslation.ca/sysrev/articles/project51/Stucki2005.pdf A conceptual framework for the OECD Health Care Quality Indicators Project. Onyebuchi A. Arah 1 , 2 , Gert P. Westert 2 , 3 , Jeremy Hurst 4 and Niek S. Klazinga 1 http://intqhc.oxfordjournals.org/content/18/suppl_1/5.full Post-Acute and Long-Term Care Reform / Estimating the Federal Budgetary Effects of the AHCA/NCAL/Alliance Proposal http://www.ahcancal.org/research_data/funding/Documents/Post%20Acute%20and%20Long%20Term%20Care%20Reform.pdf Long-Term and Post-Acute Care Financing Reform Proposalhttp://www.ahcancal.org/advocacy/Documents/FinancingReformProposal.pdf http://www.docstoc.com/docs/49810609/Summary-of-Issues-Affecting-Post-Acute-and-Long-Term La faillite sanitaire des Etats Unis – Bertrand Kiefer au sujet du rapport: U.S. Health in International Perspective: Shorter Lives, Poorer Health http://www.nap.edu/openbook.php?record_id=13497&page=1 Le rapport: http://obssr.od.nih.gov/pdf/IOM%20Report.pdf Effectiveness of case management and post-acute services in older people after hospital discharge. Wen K Lim, Sue F Lambert and Len C Gray. Med J Aust 2003; 178 (6): 262-266. Cherilyn G Murer: A Patient-Centered Vision for Post-Acute Care Reform http://murer.com/pdfs/articles/vision4post-acutecarereform-mar07.pdf |
| Payments basics (MEDPAC) Home health care services payment system 10/14/2016 Document Type: Payment Basics Hospice services payment system 10/14/2016 Document Type: Payment Basics Inpatient rehabilitation facilities payment system 10/14/2016 Document Type: Payment Basics Long-term care hospitals payment system 10/14/2016 Document Type: Payment Basics Skilled nursing facility services payment system 10/14/2016 Document Type: Payment Basics | Une réforme des soins post-aigus est en cours vers un système uniforme de données et de paiement.Post-Acute Quality Initiatives: The Continuity Assessment Record and Evaluation (CARE) Item SetIRF – PAI (Inpatient Rehabilitation Facilities)MDS 3.0 (Skilled Nursing Facilities, …)Aux USA outils de recueil et de tarification sont différents selon le type de soins post-aigus |
Extrait d’un texte de Carl Granger: « Like acute medical management, functional restoration requires intensive rehabilitation that is costly but time-limited and episodic. In contrast, long-term care requires an ongoing but lower daily investment of therapy and care-giving services. Among those with the capacity for functional restoration, an episodic payment approach such as an FRG-based PPS would tend to encourage timely discharge from the SNF to the community. In contrast, a per diem rate adjusted for severity of disability may provide financial incentives to maintain residents in their most dependent state. Although a unified payment system has appeal, its development presents challenges. One approach might combine elements of an episode-based system for short-term restorative-level rehabilitation patients within a larger per diem-based scheme. »
Une mise au point sur l’histoire du paiement prospectif en réadaptation (MDS-PAC vs. FIM): Deciphering the details: an update of implementing PPS for inpatient rehabilitation facilities – Cherilyn G. Murer http://www.murer.com/files/uploads/docs/decipheringthedetails.pdf Comprendre les FIM-FRG – Function-related Group Classification and Case-mix Adjustment (Carl Granger et al.) http://emedicine.medscape.com/article/317865-overview#aw2aab6b6
Paiement prospectif en soins post-aigu aux USA Les PPS à l’activité (« fee-for-service ») ont été mis progressivement en place, en 1998 pour les Skill Nurse Facilities (SNF) et 2002 pour les Inpatient Rehabilitation Facilities (IRF) l’ordre chronologique des articles retrace l’histoire de leur mise en oeuvre et des débats associés. 1994 – A case-mix classification system for medical rehabilitation, 1994, vol. 32, n° 4. – p. 366-379 Auteur(s) : Stineman, Margaret G. ; Escarce, J.J. ; Goin, J.E. ; Hamilton, B.B. ; Granger, C.V. ; Williams, S.V. Résumé : Dissatisfaction with Medicare’s current system of paying for rehabilitation care has led to proposals for a rehabilitation prospective payment system, but first a classification system for rehabilitation patients must be created. Data for 36,980 patients admitted to and discharged from 125 rehabilitation facilities between January 1, 1990, and April 19, 1991, were provided by the Uniform Data System for Medical Rehabilitation. Classification rules were formed using clinical judgment and a recursive partitioning algorithm. The Functional Independence Measure version of the Function Related Groups (FIM-FRGs) uses four predictor variables: diagnosis leading to disability, admission scores for motor and cognitive functional status subscales as measured by the Functional Independence Measure, and patient age. The system contains 53 FRGs and explains 31.3% of the variance in the natural logarithm length of stay for patients in a validation sample. The FIM-FRG classification system is conceptually simple and stable when tested on a validation sample. The classification system contains a manageable number of groups, and may represent a solution to the problem of classifying medical rehabilitation patients for payment, facility planning, and research on the outcomes, quality, and cost of rehabilitation. Voici une réflexion de Carl Granger en 1997 avant la mise en place des PPS en soins post-aigus, bien connu pour la Mesure de l’Indépendance Fonctionnelle, moins connu pour ses écrits sur les systèmes de tarification. Cela semble bien répondre à notre problématique française des programmes de réadaptation intensive et multidiciplinaire. 1997 – A modular case-mix classification system for medical rehabilitation illustrated – Innovations in Fee-For-Service Financing and Delivery by Margaret G. Stineman, Carl V. Granger http://findarticles.com/p/articles/mi_m0795/is_n1_v19/ai_20750871/?tag=mantle_skin;content
1997 – Testimony on Rehabilitation & Long-Term Care Hospital Payments by Barbara Wynn Acting Director, Bureau of Policy Development Health Care Financing Administration U.S. Department of Health and Human Services http://www.hhs.gov/asl/testify/t970410b.html 1997 Medicare reimbursement system encourages increased payments to rehabilitation hospital http://www.washington.edu/news/archive/id/2957
2006 – Changes in the Use of Postacute Care during the Initial Medicare Payment Reforms Does It Matter? Wen-Chieh Lin, Robert L Kane, David R Mehr, Richard W Madsen, and Gregory F Petroski
2009 – The End of Fee-for-Service Medicine? Proposals for Payment Reform in Massachusetts NEJM | July 29, 2009 | Topics: Cost of Health Care, Medicare and Medicaid http://healthpolicyandreform.nejm.org/?p=1247
http://murer.com/pdfs/articles/PostAcuteCareBundlingPlan-July09.pdf 2009 – Inpatient rehabilitation facilities under the prospective payment system: lessons learned. Zorovitz RD. Eur J Phys Rehabil Med. 2009 Jun;45(2):259-63.
Change in inpatient rehabilitation admissions for individuals with traumatic brain injury after implementation of the medicare inpatient rehabilitation facility prospective payment system. http://www.ncbi.nlm.nih.gov/pubmed/22840827#
Autres documents étrangers
Réformes du système de santé, intégration verticale, substituabilité et buffer management en soins post-aigus
Voir aussi la page « Qui a peut de l’intégration des soins? » – Chapitre consacré aux soins post-aigus et à la réadaptation
USA – Pays Bas – France: effets des paiements prospectifs, intégration verticale, substituabilité des orientations, résultats cliniques…
| Shorter Length of Stay Is Associated With Worse Functional Outcomes for Medicare Beneficiaries With Stroke Suzanne R. O’Brien, Ying Xue, Gail Ingersoll† and Adam Kelly – Physical Therapy December 2013 vol. 93;no. 12 1592-1602 2004 Trends in Length of Stay, Living Setting, Functional Outcome, and Mortality Following Medical Rehabilitation (en fulltext) Kenneth J. Ottenbacher, PhD, OTR; Pam M. Smith, DNS, RN; Sandra B. Illig, MS, RN; Richard T. Linn, PhD; Glenn V. Ostir, PhD; Carl V. Granger, MD JAMA. 2004;292:1687-1695. 2005 Effects of Payment Changes on Trends in Access to Post-Acute Care – Abstract – Site Melinda Beeuwkes Buntin, José J. Escarce, Carrie Hoverman, Susan M. Paddock, Mark Totten, Barbara O. WynnSupported by the Centers for Medicare and Medicaid2006 Changes in the Use of Postacute Care during the Initial Medicare Payment Reforms Does It Matter? – Autre lien Wen-Chieh Lin, Robert L Kane, David R Mehr, Richard W Madsen, and Gregory F Petroski – HSR: Health Services Research 41:4, Part I (August 2006) « The shift in usage among settings occurred in two stages that corresponded to the timing of payment reforms for home health agencies and SNFs. Evidence strongly suggests the substitutability between PAC settings. Financial incentives, in addition to clinical needs and individual preferences, play a major role in PAC use. » Voir SUBSTITUTABILITY ACROSS INSTITUTIONAL POST-ACUTE CARE SETTINGS: 1998-2006 (US department of Health & Human Services) 2008 – Medicare’s new restrictions on rehabilitation admissions: impact on the elderly. Segal M, Pedersen AL, Freeman K, Fast A: Medicare’s new restrictions on rehabilitation admissions. Am J Phys Med Rehabil 2008;87:872-882. Department of Physical Medicine and Rehabilitation, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, New York 10467, USA.
2009 Les hôpitaux français face au paiement prospectif par cas. Gérard de Pouvourville. La mise en oeuvre de la T2A (2009)
2013 Post-acute care and vertical integration after the Patient Protection and Affordable Care Act. (2013)
https://www.ache.org/chapters/downloads/chapter_education/materials_template79B.pdf |
http://www.aha.org/research/reports/tw/10nov-tw-postacute.pdf
Bundling et soins post-aigus
« Obamacare »: Effets potentiels sur la MPR aux USA
Bundling Acute and Postacute Payment: From a Culture of Compliance to a Culture of Innovation and Best Practice
| Model 1: Hospital services provided to a beneficiary during an acute inpatient stay, where physicians are partners in improving care Model 2: Hospital, physician, post-acute provider, and other Medicare-covered services provided during the inpatient stay as well as during recovery after discharge to the home or another care setting Model 3: Hospital, physician, post-acute provider, and other Medicare-covered services beginning with the initiation of post-acute care services after discharge from an acute inpatient stay Model 4: CMS would make a single, prospectively determined bundled payment to the hospital that would encompass all services furnished during the inpatient stay by the hospital, physicians and other practitioners. Physicians and other practitioners would submit “no-pay” claims to Medicare and would be paid by the hospital out of the bundled payment (2) |
Bundled payments – paiments regroupés
Lessons Learned: Implementation of Prometheus Payment Initiative Septembre 2012 Testing PROMETHEUS Payment® A payment model uses Evidence-informed Case Rates® to meet health care needs Septembre 2012 BUNDLED PAYMENT ACROSS THE U.S. TODAY: Status of Implementations and Operational Findings Novembre 2011 Analysis of HEALTHCARE Interventions That Change Patient Trajectories. 2005
Geisinger Health System
|
Le paiement « au parcours » (bundled payments) et ses conséquences possibles sur les soins post-aigus
Post-acute care and vertical integration after the Patient Protection and Affordable Care Act. Shay Patrick D., MIck Stephen S. Journal of Healthcare Management. Janvier 2013
SRATEGIES FOR HEALTH CARE LEADERS Volume 71 Summer 2012 – CAIN BROTHERS Emerging Trends in Post-Acure-Care : Controlling Costs and Enhancing Quality through Collaboration By Roderick Rivera and Ejaz Elahi Dresner Partners
ACG Chicago. Avril 2010
Research and trends (AHA) Healthcare Finance News Healthcare Reform: Impact on Hospitals (HEALTH CAPITAL CONSULTANTS)
Healthcare IT in the Post-Acute Market (DUFF & PHELPS)
« Obamacare »: Effets potentiels sur la MPR aux USA Patient Protection and Affordable Care Act: An Overview &Potential Effects on PM & R – Leighton Chan, MD, MPH Chief, RMD, NIH CC
Position de l’American Academy of PM&R à propos du paiement par épisodes (page 4: questions clés)
http://www.aapmr.org/advocacy/health-policy/federal/documents/house-means-medicare-reform-letter.pdf
Post-acute care bundling plans – Cherilyn G. Murer (Cet article évoque les bundle payments à l’étude entre court séjour et psot-aigu et les propositions de l’AAPM&R)
Exploring Episode-Based Approaches for Medicare Performance Measurement, Accountability and Payment Février 2009 (voir schéma des parcours de soins) Final Report. Cheryl l. Damberg, Melony E. Sorbero, Peter S. Hussey, Susan Lovejoy, hangsheng liu, and ateev mehrotra
February 2009 – Assistant Secretary for Planning and Evaluation U.S. Department of Health and Human Services
Bundling Acute and Postacute Payment: From a Culture of Compliance to a Culture of Innovation and Best Practice (Gerben Dejong) |
| Model 1: Hospital services provided to a beneficiary during an acute inpatient stay, where physicians are partners in improving care Model 2: Hospital, physician, post-acute provider, and other Medicare-covered services provided during the inpatient stay as well as during recovery after discharge to the home or another care setting Model 3: Hospital, physician, post-acute provider, and other Medicare-covered services beginning with the initiation of post-acute care services after discharge from an acute inpatient stay Model 4: CMS would make a single, prospectively determined bundled payment to the hospital that would encompass all services furnished during the inpatient stay by the hospital, physicians and other practitioners. Physicians and other practitioners would submit “no-pay” claims to Medicare and would be paid by the hospital out of the bundled payment (2) |
FIM ou MDS-PAC (Minimum Data Set)
Evaluating the planned substitution of the minimum data set-post acute care for use in the rehabilitation hospital prospective payment system. Buchanan JL, Andres PL, Haley SM, Paddock SM, Zaslavsky AM. http://www.ncbi.nlm.nih.gov/pubmed/14734953 An assessment tool translation study by Joan L. Buchanan, Patricia L. Andres, Stephen M. Haley, Susan M. Paddock, Alan M. Zaslavsky
Comparaisons des systèmes d’orientation entre quelques systèmes étrangers
Le contenu ci-dessous est transféré sur la page pertinence des admissions et hospitalisations en SSR Le problème des systèmes d’orientation en soins post-aigu est la « substituabilité » des orientations. En témoigne, entre autres papiers, cette étude américaine:
« The shift in usage among settings occurred in two stages that corresponded to the timing of payment reforms for home health agencies and SNFs. Evidence strongly suggests the substitutability between PAC settings. Financial incentives, in addition to clinical needs and individual preferences, play a major role in PAC use. » Nous présentons rapidement ici la diversité des systèmes d’orientation d’après un rapport du centre fédéral d’expertise belge de 2007. L’importance d’un outil de recueil commun et fondé sur des indicateurs robustes apparaît capitale au regard des risques induits par les réformes du financement (paiements prospectifs par cas et bundled payments). Des effets inattendus peuvent doivent être analysés et prévenus en terme
- d’intégration verticale et horizontale
- de re-spécification (division horizontale des activités post-aiguës, hospitalières et ambulatoires) et de substituabilité du choix d’orientation entre les types d’activités, en lien avec les modes de gouvernance (décentralisation et niveaux des décisions)
- de gestion des durées de parcours hospitaliers par les techniques de « buffer management » (séjours prolongés et impasses hospitalières ou « bed blockers »)
Tiré de: Kiekens C, Van Rie K, Leys M, Cleemput I, Smet M, Kesteloot K, et al. Organisation et financement de la réadaptation locomotrice et neurologique en Belgique. Health Services Research (HSR). Bruxelles: Centre fédéral d’expertise des soins de santé (KCE); 2007. KCE reports 57B Chapitre 8 cliquer ici
Tiré de: Kiekens C, Van Rie K, Leys M, Cleemput I, Smet M, Kesteloot K, et al. Organisation et financement de la réadaptation locomotrice et neurologique en Belgique. Health Services Research (HSR). Bruxelles: Centre fédéral d’expertise des soins de santé (KCE); 2007. KCE reports 57B – Chapitre 8 cliquer ici
Webographie: pertinence des admissions / systèmes d’orientation en SSR
Patients Hospitalized for Medical Conditions in Winnipeg, Canada: Appropriateness and Level of Care
- · The preadmission screening system should collect information necessary to identify reimbursement requirements and demographic information for planned and actual admissions.
- · Clinical indicators that will assist preadmission reviewers evaluate patients against established criteria of medical appropriateness, with appropriateness information available to physicians on a “just in time” basis.
- · The preadmission system should have the ability to follow patients through the preadmission process and report on any unmet requirements, particularly tied to compliance.
- · The preadmission system should provide volume and dollar values of denials by insurers to report on the effectiveness of preadmission screening. »
Long-Term and Post-Acute Care Financing Reform Proposal